Spironolactone & POTS: Unpacking The Complex Relationship
Table of Contents
- Understanding POTS: A Complex Autonomic Disorder
- Spironolactone: More Than Just a Diuretic
- The Aldosterone Connection: Spironolactone and Fluid Balance
- The Intersection: Spironolactone and POTS – A Delicate Balance
- Patient Experiences and Anecdotes with Spironolactone and POTS
- Navigating Treatment: Alternatives and Cautions
- The Importance of Expert Guidance in POTS Management
- Future Directions in POTS Research and Treatment
Understanding POTS: A Complex Autonomic Disorder
Postural Orthostatic Tachycardia Syndrome (POTS) is a form of dysautonomia, a disorder of the autonomic nervous system (ANS), which controls involuntary bodily functions like heart rate, blood pressure, digestion, and temperature regulation. This condition is estimated to impact between 1,000,000 and 3,000,000 Americans, and millions more around the world, making it a significant public health concern. POTS is characterized by an orthostatic increase in the heart rate of ≥30 beats per minute within 10 minutes of standing or during head-up tilt, in the absence of orthostatic hypotension. For adolescents, the diagnostic criterion is an increase of ≥40 bpm. POTS is defined as the presence of chronic symptoms of orthostatic intolerance (at least 6 months) accompanied by this significant heart rate increase. Patients often experience a wide array of symptoms that worsen upon standing and improve with lying down. These can include severe fatigue, lightheadedness, dizziness, presyncope (feeling faint), syncope (fainting), brain fog, palpitations, chest pain, shortness of breath, gastrointestinal issues, and exercise intolerance. The underlying pathophysiologic mechanisms of POTS are diverse and include hypovolemia (low blood volume), sympathetic hyperactivity, peripheral denervation, and mast cell activation, among others. This clinical heterogeneity means that what works for one POTS patient may not work for another, necessitating highly individualized treatment approaches.Spironolactone: More Than Just a Diuretic
Spironolactone is a generic prescription tablet widely recognized for its role in treating high blood pressure and various other conditions. It is available under brand names like Aldactone and CaroSpir. To understand its potential implications for POTS, it's essential to first grasp its primary functions and mechanisms.What is Spironolactone and How Does It Work?
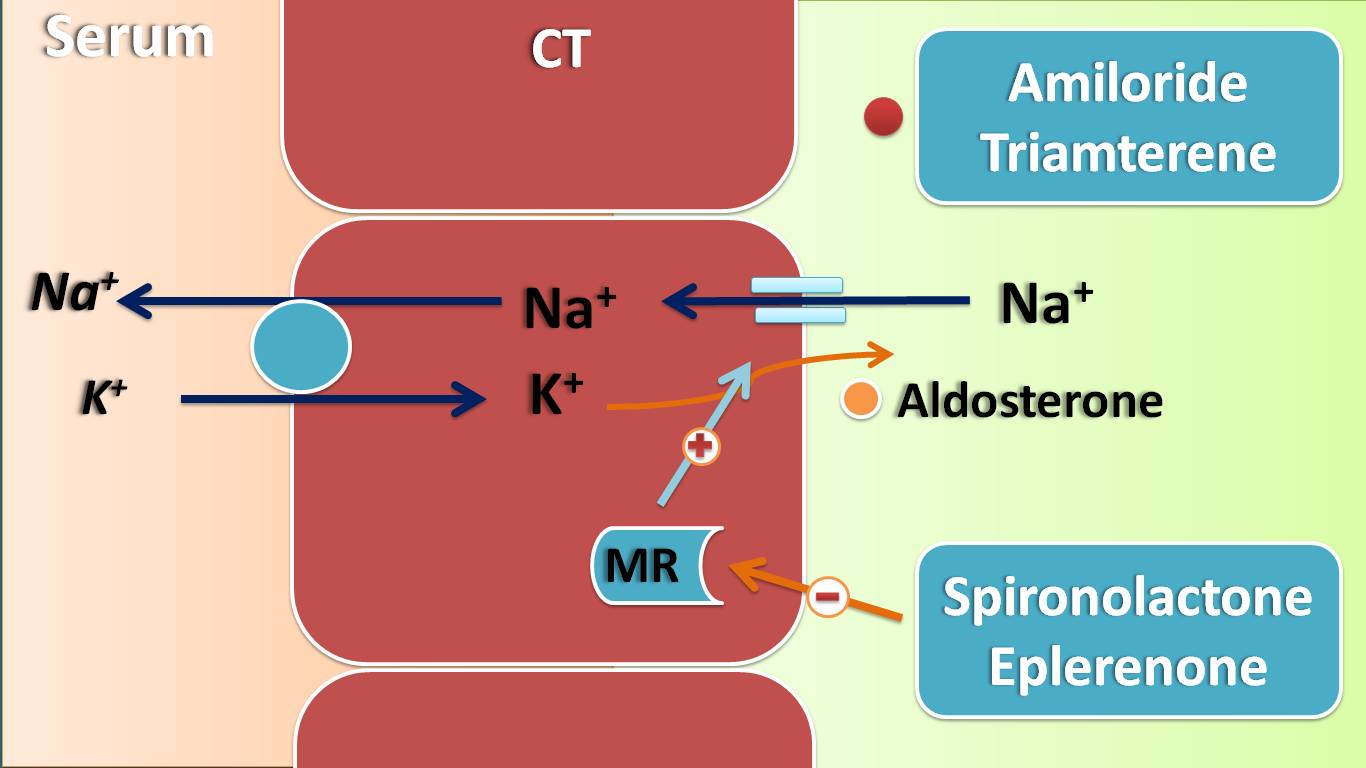
At its core, spironolactone is a diuretic, often referred to as a "water pill," that helps the kidneys remove more fluid from the body. However, unlike many other diuretics, spironolactone is unique because it is a potassium-sparing diuretic. This means it prevents your body from absorbing too much salt and, crucially, keeps your potassium levels from getting too low. This characteristic is vital, as many other diuretics can lead to hypokalemia (low potassium), which can cause serious side effects. The key to spironolactone's action lies in its ability to block the effects of aldosterone. Aldosterone is a hormone produced by the adrenal glands that plays a critical role in regulating salt and water balance in the body. By blocking aldosterone, spironolactone helps the kidneys excrete more sodium and water while retaining potassium. This mechanism makes it effective in reducing fluid retention and lowering blood pressure.Common Uses of Spironolactone
Spironolactone is frequently prescribed for conditions such as heart failure, high blood pressure, and fluid retention (edema) related to heart, kidney, or liver disease. In heart failure, it helps by blocking the effects of aldosterone, which prevents damage to heart tissues and improves overall heart function. Lowering high blood pressure helps prevent strokes and heart attacks. Additionally, spironolactone is used to treat certain patients with hyperaldosteronism, a condition where the body produces too much aldosterone. Its versatility makes it a valuable medication in various clinical scenarios.The Aldosterone Connection: Spironolactone and Fluid Balance
The role of aldosterone in the body's fluid and electrolyte balance is profound. Aldosterone promotes sodium and water reabsorption in the kidneys, leading to increased blood volume and blood pressure. In conditions like heart failure, excessive aldosterone can contribute to fluid overload and cardiac remodeling. By acting as an aldosterone antagonist, spironolactone directly counteracts these effects, leading to diuresis (increased urine production) and a reduction in fluid volume. This mechanism is generally beneficial for conditions where fluid retention is a problem. However, for individuals with POTS, where hypovolemia (low blood volume) is a common contributing factor, altering fluid balance can be a double-edged sword. While some POTS patients might experience fluid retention, many others struggle with maintaining adequate blood volume, which is essential for blood pressure regulation upon standing.The Intersection: Spironolactone and POTS – A Delicate Balance
The question of using spironolactone in POTS patients is complex and often debated within the medical community. Given its mechanism of action, one might intuitively think that a diuretic could worsen the hypovolemia often seen in POTS. However, some specific subtypes of POTS, particularly those with hyperadrenergic features or elevated aldosterone levels, might theoretically benefit from its effects.Potential Considerations for Spironolactone in POTS
In certain rare cases, where a POTS patient might exhibit characteristics like high blood pressure alongside fluid retention, or perhaps a specific form of hyperaldosteronism contributing to their symptoms, spironolactone might be considered. The idea would be to modulate fluid and electrolyte balance in a way that stabilizes blood pressure and reduces sympathetic overdrive. However, this is not a common or first-line approach for most POTS patients. The "Data Kalimat" mentions that "Spironolactone is frequently prescribed for conditions such as heart failure, high blood pressure, and fluid retention (edema)," but it does not list POTS as a frequent indication, underscoring its limited, if any, role in general POTS management.Why Spironolactone Might Be Problematic for POTS Patients
Despite any theoretical benefits in highly specific scenarios, for individuals with POTS, using spironolactone requires careful consideration, and in many cases, it could be detrimental. The primary concern revolves around its diuretic effect. Many POTS patients already struggle with low blood volume (hypovolemia), which contributes significantly to their orthostatic symptoms. "O drospirenone is a spironolactone analog that could worsen hypovolemia," and this principle applies directly to spironolactone itself. By increasing fluid excretion, spironolactone can exacerbate existing hypovolemia, leading to a further drop in blood pressure upon standing and a compensatory increase in heart rate. This could worsen orthostatic intolerance and intensify symptoms like dizziness, lightheadedness, and fatigue. Furthermore, spironolactone acts as an aldosterone antagonist, and this action can complicate the delicate neurohormonal balance in POTS. While aldosterone regulation can be complex in POTS, widespread diuresis generally runs counter to the goal of increasing blood volume, which is a cornerstone of POTS management (e.g., through increased fluid and salt intake). The statement "🤪 so essentially horrible in combo with POTS" from the provided data, while informal, captures the sentiment of many patients and clinicians regarding the potential negative impact of spironolactone on POTS symptoms. Other medications that might predispose to tachycardia, such as diuretics, vasodilators, tricyclic antidepressants (TCAs), and selective norepinephrine reuptake inhibitors (SNRIs), are often withdrawn or used with extreme caution in POTS patients precisely because they can worsen the characteristic heart rate increase upon standing. Spironolactone, being a diuretic, falls into this category of medications that could potentially worsen tachycardia and overall orthostatic intolerance.Patient Experiences and Anecdotes with Spironolactone and POTS
Anecdotal evidence from patient communities often highlights the challenges of managing POTS with medications not specifically designed for it. A number of POTS patients report varied experiences with different treatments. While some people find success with spironolactone for its intended uses (like PCOS, as mentioned in one data point: "My sister has POTS and we are pretty sure i have a predisposition based on some similar characteristics, I got prescribed spiro for my pcos which dumps potassium into your body and."), its effects on POTS symptoms are often negative. The online community "A place for anyone on a spironolactone journey to ask questions, share their story, and discuss anything related to spironolactone" might include discussions about its impact on co-occurring conditions like POTS, where experiences are likely to lean towards caution. The general consensus among many patients and specialists is that medications that deplete fluid volume are typically counterproductive for POTS.Navigating Treatment: Alternatives and Cautions
Given the potential for spironolactone to worsen POTS symptoms, especially hypovolemia and tachycardia, healthcare providers typically explore other treatment avenues. Management strategies for POTS often focus on increasing blood volume through high fluid and salt intake, wearing compression garments, and implementing a structured exercise program. Pharmacological interventions commonly include fludrocortisone (which helps the body retain salt and water), midodrine (a vasoconstrictor), beta-blockers (to lower heart rate), and sometimes pyridostigmine or ivabradine, depending on the patient's specific POTS subtype and symptoms. When considering diuretics, if fluid retention is truly an issue in a POTS patient, careful selection is paramount. Drospirenone, a spironolactone analog, is mentioned as potentially worsening hypovolemia, highlighting the general risk with this class of drugs for POTS. While spironolactone and eplerenone are comparably effective as aldosterone antagonists, their structure/function relationships and metabolite/half-life considerations provide the basis for differentiating these drugs, but the fundamental concern about diuresis remains for POTS patients. It's crucial for patients to openly discuss all medications, including over-the-counter drugs and supplements, with their doctor. As the data suggests, "In addition to potential side effects, spironolactone can interact with certain foods and" other medications, making a comprehensive review essential.The Importance of Expert Guidance in POTS Management
POTS is a clinically heterogeneous disorder with multiple contributing pathophysiologic mechanisms. This complexity underscores the critical need for diagnosis and management by healthcare professionals experienced in autonomic disorders. Self-medicating or adjusting prescribed medications based on anecdotal evidence can be dangerous, particularly with conditions like POTS that involve delicate physiological balances. A physician will assess the individual's specific POTS subtype, co-existing conditions, and overall health profile before considering any medication. They will weigh the potential benefits against the risks, closely monitor the patient's response, and adjust treatment as necessary. For instance, if a patient with POTS also has a condition like PCOS for which spironolactone is typically prescribed, the doctor would need to carefully consider the potential interactions and prioritize the most impactful symptoms or conditions. The "Learn about its side effects, uses, dosage, and more" and "Find patient medical information for spironolactone (aldactone, carospir) on WebMD including its uses, side effects and safety, interactions, pictures, warnings, and user" points emphasize the wealth of information available, but this information should always be interpreted and applied under medical supervision.Future Directions in POTS Research and Treatment
The understanding of POTS continues to evolve. Research into its various subtypes and underlying mechanisms is ongoing, with efforts to identify more targeted and effective treatments. The search for similar cases via online databases like PubMed, Scopus, and Cochrane helps researchers identify patterns and potential new therapeutic avenues. For example, studies on "orthostatic symptoms and reductions in cerebral blood flow in long-haul COVID-19 patients" show similarities with myalgic encephalomyelitis/chronic fatigue syndrome, highlighting the interconnectedness of various complex conditions and the potential for shared treatment insights. As our knowledge of POTS deepens, more precise and safer treatment options will likely emerge, reducing the reliance on medications with potentially conflicting effects like spironolactone. In conclusion, while spironolactone is a valuable medication for conditions like hypertension, heart failure, and edema, its role in the management of Postural Orthostatic Tachycardia Syndrome is generally limited and often contraindicated due to its diuretic effects and potential to worsen hypovolemia and tachycardia. The complex nature of POTS demands an individualized, cautious, and expert-guided approach to treatment. If you are a POTS patient and spironolactone has been mentioned in your treatment plan, or if you have any concerns about your current medications, it is imperative to have an open and thorough discussion with your healthcare provider. Your journey to managing POTS effectively is best navigated with informed medical guidance.What are your experiences with spironolactone or other diuretics in the context of POTS? Share your thoughts and questions in the comments below, or consider sharing this article with others who might benefit from this discussion.
Potassium sparing diuretics – Mechanism and actions

Effectiveness of spironolactone for women with acne vulgaris (SAFA) in

Spironolactone Oral Suspension, 25 mg/5 mL - Padagis